![]()
If HEALTHCAREfirst provides billing services to your agency, you do not need to do anything. We will manage this setup for you.
HEALTHCAREfirst is changing Network Service Vendors and is now partnered with the ABILITY Network. The transition has already occurred and requires prompt attention from your organization in order to ensure there no delays in cash flow or with your billing process. Your agency must take action in firstHOMECARE and/or firstHOSPICE to continue:
● Creating and submitting electronic claims
● Downloading claims for submission
● Receiving response files
We have outlined a step-by-step process to guide you through everything that needs to occur in order for you to make this transition smoothly. Step one is required by all agencies regardless of whether you wish to enroll in firstREV.
|
|
If HEALTHCAREfirst provides billing services to your agency, you do not need to do anything. We will manage this setup for you. |
1. Setup Receiver IDs for all Receivers and associate them to offices BEFORE your transition date. firstHOMECARE and firstHOSPICE clients will be migrated based on the MAC jurisdiction you reside in. Login the day after migration to ensure your receiver IDs are properly associated with your payors. This step is required in order to submit claims going forward.
2. Determine if you wish to transition to firstREV. We are including these services to you at no additional charge for being a valued customer. There are many benefits of switching as outlined on page 6.
3. Start firstREV enrollment process. Steps 3-5 are optional.
4. Enroll with payors that require additional enrollment.
5. Register for training on firstREV.
Continue reading to find detailed instructions for each step!
For answers to your most pressing questions, refer to the firstREV FAQ topic.
Step 1: Receiver ID Setup, Office and Payor Association (REQUIRED)
Receiver IDs must be set up in firstHOMECARE and/or firstHOSPICE prior to your transition date, in order to create claims, send claims, and receive responses going forward.
Before your transition date, set up Receiver IDs and associate them to offices:
1. Navigate to Master Files | Receivers.
2. Click New
3. Enter your Receiver and Submitter data. Reference the MAC Jurisdictions and Receiver IDs on page 3 and the commonly used Commercial/Medicaid Receiver IDs found on page 5
4. Click Save
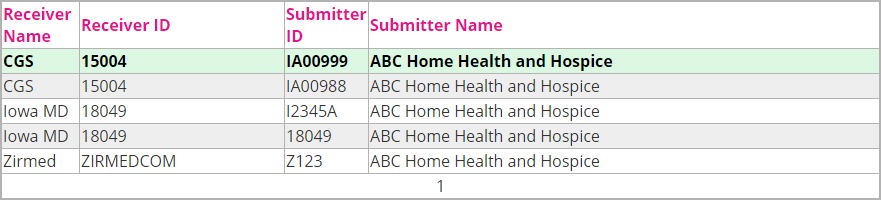
5. Repeat steps 1-4 for each Receiver you use for electronic submission. If you have more than one submitter ID per Receiver, create one Receiver record for each. Example: ABC HH&H electronically submits to CGS for Medicare, Iowa for Medicaid, and Zirmed for commercial
After your transition date, verify that payors and offices are associated to your Receiver IDs:
1. Navigate to Master Files | Payor/Plans.
2. Select a payor that is submitted electronically. Ensure that Send Electronic 837 Bill is checked
3. Verify the Receiver ID selected in the drop-down is correct. If there is no receiver ID selected (or the incorrect one is selected), select the receiver ID that the corresponding payor is associated with and then click Save.
4. Repeat steps 1-3 for all payors that are submitted to electronically.
If your non-Medicare receiver ID records are only associated to one submitter number/location each, no further action is needed. HEALTHCAREfirst will associate them and any Medicare receiver ID records to your offices upon the corresponding transition date for your agency's jurisdiction.
Step 1: Continued...
If any of your non-Medicare Receiver ID records are associated to multiple submitter numbers/locations, please go to Master files | Agency | Electronic Submitters and associate your offices to the correct submitter number/Receiver ID record.
1. Navigate to Master Files | Agency.
2. Select your first office record.
3. Click on the Electronic Submitter tab.
4. Check the Use box next to the applicable receiver record.
5. Click Save.
6. Repeat steps 1-4 for each office that has its own Receiver ID/Submitter number record.
Agencies will be transitioned using the schedule and dates listed below:
Wave 1 – April 11
● Jurisdiction K Clients – NGS – ID 14011
o States: Connecticut, Maine, Massachusetts, New Hampshire, New York, Rhode Island, Vermont
Wave 2 – April 18
● Jurisdiction 6 Clients – NGS – ID 06001
o States: Michigan, Minnesota, New Jersey, New York, Puerto Rico, US Virgin Islands, Wisconsin
● Jurisdiction 6 Clients – NGS – ID 06014
o States: Alaska, American Samoa, Arizona, California, Guam, Hawaii, Idaho, Nevada, Northern Mariana Islands, Oregon, Washington
Wave 3 – April 20
● Jurisdiction 15 Clients – CGS – ID 15004
o States: Colorado, Delaware, District of Columbia, Iowa, Kansas, Maryland, Missouri, Montana, Nebraska, North Dakota, Pennsylvania, South Dakota, Utah, Virginia, West Virginia, Wyoming
Wave 4 – April 24
● Jurisdiction M Clients – Palmetto GBA – ID 11001
o States: Arkansas, Alabama, Florida, Georgia, Illinois, Indiana, Kentucky, Louisiana, Mississippi, New Mexico, North Carolina, Ohio, Oklahoma, South Carolina, Tennessee, Texas
Step 2: Determine Whether to Use firstREV
firstREV is an optional feature offered at no additional cost that allows you to manage your entire revenue cycle for all payors. There are many benefits of using firstREV, as outlined in the section at the end of this topic. You will gain greater visibility to claims and you will have more utility at your fingertips. Additionally, you may be able to eliminate the cost of your current clearinghouse, saving money for your agency. All you have to do to get started is enroll!
Please note that it is not necessary for your agency to use firstREV, as you will still be able to send Medicare claims and receive responses within the system without it. For other payors, you will still be able to generate the 837 claim file, download it to your computer, and then upload it to your payor. However, the ability to edit claims directly on the UB04 will be moving to firstREV.
Step 3: Start Enrollment Process (OPTIONAL)
To get started with firstREV, agencies will need to complete an onboarding process. The first step is to complete the enrollment form/report. To make this process easy, HEALTHCAREfirst has created a report in the software that contains almost all of the information needed. Please note that this report will not be available for your agency until after your transition date (outlined in the "Step 1: Continued" section above).
1. Navigate to Reports | Master Listing.
2. Click firstREV Enrollment Report.
3. Review all of the information in this report to confirm its accuracy, add in any missing information, and then save this file to your computer.
4. E-mail your approved firstREV Enrollment report to firstrevsupport@healthcarefirst.com.
Step 4: Additional Payor Specific Enrollment
Some payors require additional enrollment forms to be completed. HEALTHCAREfirst will determine if your payors have additional enrollment requirements and send you any additional enrollment forms that need to be completed. It is important to complete them fully not leaving anything blank as this may result in a denial of enrollment. Please send additional payor-specific enrollment forms to firstrevsupport@healthcarefirst.com. Your prompt response will expedite account setup.
HEALTHCAREfirst will respond back to you as soon as we have more information regarding your set up. Payor responsiveness varies so please be patient during this time. Note that you can continue to submit claims to these payors just as you always have in the past by generating the 837 claim file from the HEALTHCAREfirst system and uploading directly to your payor or send by your normal process. By enrolling with the payor through firstREV, you will no longer be uploading to them through another clearinghouse, so you may want to cancel any contractual relationships once you are live in firstREV.
Step 5: Training
HEALTHCAREfirst will be offering the following webinars to get you up to speed quickly and answer your questions. Webinars will be recorded so if you miss it, don’t worry! We’ll send you a link to the recorded webinar. This is a full featured system with a lot of utility enabling you to effectively manage your revenue cycle like never before. We know you’re going to love it!
firstREV Basics
Tuesday, April 18 | 1:00pm-2:00pm CT | Register Here
Wednesday, April 26 | 10:00am-11:00am CT | Register Here
Tuesday, May 9 | 10:00am-11:00am CT | Register Here
Commonly Used Commercial and Medicaid Receiver IDs
● HEW = 810525733
● Availity = 030240928
● WebMD/Emdeon= 133052274
● Highmark = 54771
● Highmark Senior = 15460
● MDOnline = MCC
● Zirmed = ZIRMEDCOM
● Office Ally = 330897513
● UHIN Medicaid FFS = HT000004-001
● UHIN Medicaid MCO = HT000004-002
● UHIN Medicaid DVP = HT000004-00)
● UHIN Medicaid Crossovers = HT000004-005
● UHIN Medicaid Atypical = HT000004-801
● Aetna = 042064683
● Relay Health = CLAIMSCH
● Louisiana Medicaid = LA-DHH-
● Texas Medicaid =617591011CMSP
● Ohio Medicaid = MMISODJFS
● Connecticut Medicaid = 061274678
● Medi-Cal (CA Medicaid) = 610442
● Iowa Medicaid = 18049
● NC Medicaid = DNC00
● Mass Health = DMA7384
Benefits of Using firstREV
firstREV is a smarter way for home health and hospice providers to manage their entire revenue cycle. From submitting all payor claims electronically, checking eligibility, managing appeals and the remittance process, agencies will have total visibility to every aspect of the claim lifecycle with 100% acknowledgement on all transactions making it easier than ever to pinpoint billing issues and resolve problems quickly. With superior claim scrubbing and more complete documentation, firstREV helps eliminate administrative burdens and improve the bottom line.
HEALTHCAREfirst partners with ABILITY Network to link directly to source data to bring you faster transaction processing, higher first-pass acceptance rates and superior denials management in an easy to use interface. Everything you need to seamlessly bill for all payors is fully integrated so you never have to leave the software!
Significantly decrease payor rejections – Get first-pass payor acceptance rates of 98% or better.
Gain greater visibility into claims status - Users receive all messages from the payer, always tied to the original claim and for the life of the claim until reimbursed.
Receive fast, clear correction guidance - Any claim rejected by a payer is instantly placed back in the work queue with a clear message about the correction needed - no more waiting and wondering!
Reduce A/R days – Speed up the payment cycle by validating claims against the most current rules available.
Work more efficiently – Work with individual transactions or in batches based on user preference, easily edit UB04 forms directly, attach notes, create your own user defined dashboard and more.
Quickly pinpoint issues – Extensive audit trail shows every detailed change made to a claim throughout its lifecycle allowing you to identify any breakdowns in the process and prevent future occurrences.
End manual, time-consuming follow-up - Fast, up-to-date correction messages stop the need for users to hunt down rejection causes, contact payers, submit appeals, and monitor “unique” payer rules.
Eliminate eligibility issues upfront – Verify eligibility at the time a claim is uploaded to flag any issues and correct them, avoiding adjudication issues.
Efficiently manage denials and appeals – Easily track and work claim appeals through final determination without leaving the software.
Customize business rules with robust rules engine – Easily customize business rules to tailor the system to your needs and stay current with even the most complicated rule sets from commercial payors and CMS.
Monitor financial performance - Robust analytics paint the entire picture of financial performance with details for addressing common issues.
Questions? Read FAQs about firstREV to learn more.
Need help? Contact our firstREV enrollment team at firstrevsupport@healthcarefirst.com.